You were injured at work and you have a workers’ compensation claim. How do you move your claim forward and try to recover compensation for your injury?
The answer, hands down, is to get medical treatment and provide all necessary medical documentation to show evidence of the medical treatment you are receiving.
Without medical treatment, not only do you risk not getting better, but you also run the risk of stalling your workers’ compensation claim. (That’s just what some insurers may be hoping for.) If you do not have proper medical documentation, it makes it easier for the workers’ compensation insurance company to try to deny you the benefits you may be entitled to.
So it is important that when the insurance company is sending you for medical treatment, you follow the doctor’s orders. This means:
- Attending all appointments as scheduled
- Taking medication as prescribed
- Communicating with the doctor about your injuries
- Following all restrictions the doctor puts you under
You may have many questions and concerns about your medical treatment after a work injury. Here are some other frequently asked questions about workers’ comp medical benefits, along with answers based on extensive experience.
Will I Miss Out on Benefits if I Don’t See a Doctor Right After My Work Injury?
While there is no strict requirement that you must see a doctor immediately after a work accident, it is generally a good idea to see one as soon as possible. Having a medical doctor evaluate your injuries after an accident offers documented proof to the insurance company and your employer that you sustained an injury. The insurance company isn’t simply going to take your word for it. Without documentation, the insurance company or your employer may not believe that you were injured and they could try to deny your claim. I’ve seen this happen.
When you go to the doctor, they will document your injuries, how and when you said you received them, and they will outline a plan of care. Make sure you explain to the doctor exactly how you were injured and tell them all of the medical problems you are having related to the injury. It is important to be clear and direct when communicating with the doctor so hopefully they can document the circumstance surrounding your injury and accident. This way, your employer and insurance company can understand exactly what happened.
What Kind of Treatment Can I Get Under Workers’ Comp Insurance?
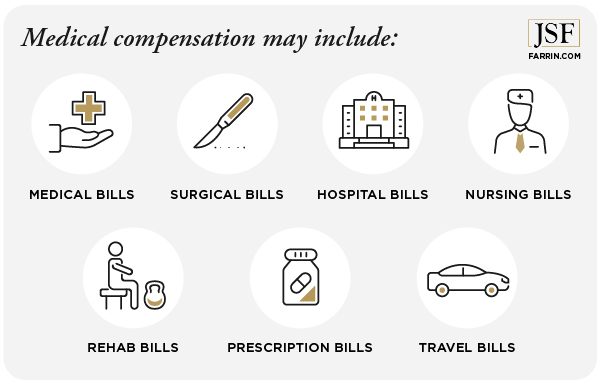
If you’re injured on the job and your workers’ compensation claim is approved, workers’ comp will pay for your medical treatment. So what is medical compensation?
Under the North Carolina Workers’ Compensation Act, “medical compensation” can include virtually anything that will cure your injury, give you relief from pain, and/or get you well enough to get back to work. Under South Carolina workers’ compensation law, employers are generally required to provide medical treatment that “will tend to lessen the period of disability.”
Medical treatment for your workers’ comp injury can include:
- Medical
- Surgical
- Hospital
- Nursing
- Rehabilitative services, such as:
- Attendant care services: At-home care or physical therapy
- Vocational rehabilitation: In some circumstances, the insurance company will pay for retraining or for a specialist to help you find another job
- Medicines
- Sick travel: Reimbursement for any travel to authorized medical providers or pharmacies 20 miles or more roundtrip in North Carolina or 10 miles in South Carolina
- Other treatment
How Do I Receive Medical Treatment for Worker’s Comp – and Who Controls It?
If you have an accepted workers’ compensation claim in North Carolina or South Carolina, you are entitled to medical benefits. This usually includes things like doctor appointments, physical therapy, prescriptions, and even surgery. Generally speaking, medical benefits for workers’ compensation are any treatments that help you recover from your injury.
In many cases, medical benefits for workers’ compensation even apply to travel costs to and from your medical appointments (if more than 20 miles round-trip in North Carolina, or 10 miles in South Carolina), attendant care, medical equipment, and home or vehicle modifications.
Unlike a typical health insurance plan, there are no co-pays or deductibles in workers’ compensation cases. The insurance company is responsible for 100% of your approved medical expenses. It sounds pretty good, right? But there’s a catch.
Who Chooses the Workers’ Compensation Doctor?
In North Carolina and South Carolina, the workers’ compensation insurance company has the right to direct your medical care. This means they choose your workers’ compensation doctors and when you see them.
If you refuse treatment, the insurance company might try to cut off your benefits altogether.
If you request a second opinion, the insurance company might deny the request or try to force you to choose from a carefully-selected workers’ compensation doctor list before agreeing to pay for it. If you choose to pay for the treatment on your own, you might not be reimbursed.
So I Have to See a Workers’ Comp Doctor? I Can’t See My Own Doctor Instead?
Here’s the deal: When an insurance company admits liability for your North Carolina workers’ compensation claim, they have the right to direct your medical care. This means they get to tell you which doctors to see and when to see them. If you go to your own doctor, the insurance company will probably refuse to pay for it. If your doctor makes any new treatment recommendations, they will probably refuse to pay for those as well. Bottom line, if you treat with your own doctor, you may end up getting stuck with the bill.
Can I Trust a Provided Workers’ Compensation Doctor?
Under North Carolina and South Carolina law, if you are injured on the job and your employer agrees to provide workers’ compensation benefits for your injury, then your employer and their insurance carrier generally have the initial right to choose the physician who will treat your injuries. Some insurance companies may want to get you back to work as quickly as possible (even if you’re not ready). This is one of the many reasons insurance companies may benefit when they direct your medical care and send you to doctors they select.
Can I Request a Second Opinion?
As an injured worker, you have the right to request to be provided with treatment from a different physician. North Carolina law allows you to petition the North Carolina Industrial Commission to obtain a second opinion if the employer and their insurance carrier will not agree. In South Carolina, that appeal would be to the South Carolina Workers’ Compensation Commission if necessary.
North Carolina
When you request a second opinion, the insurance company has 14 days to respond. North Carolina law encourages the parties to try to agree on a particular doctor during that time.
At the end of 14 days, if you still haven’t reached an agreement, you have the option of taking your request to the Industrial Commission, where an administrative judge will make the call. If your second opinion is approved, you may be able to switch over to the new doctor for the remainder of your treatment, but that process typically involves approval from the Industrial Commission.
South Carolina
In South Carolina, if you’re not happy with the treatment from your appointed physician, you can ask to see a different doctor. If that request is denied, you can file a request for a hearing before a Workers’ Compensation Commissioner for a decision.
If the insurer or employer agrees to a second opinion, they generally get to choose that doctor as well. An experienced workers’ compensation attorney can help you navigate this situation and may be able to recommend potential medical care providers for the second opinion as well.
Contact a Lawyers
If you feel that your employer sent you to a doctor that did not give you the best medical care, then you should consider contacting an attorney. An experienced workers’ compensation lawyer can make the process easier for you, while minimizing the risks of trying to handle this cumbersome and confusing process on your own.
Having Trouble Moving Your Comp Claim Forward?
Imagine this scenario: You’ve been injured on the job, and the insurance company finally accepts your claim and schedules an appointment for you with a doctor. On the day of your appointment, you spend 30 minutes in the waiting room, followed by a grand total of 30 seconds with the doctor. No one asks you how you’re feeling. No one asks whether you can safely return to work.
The very next day, the insurance company calls to tell you that you’ve been released from treatment and are expected to report to work immediately. All the while, the pain from your injury has gotten even worse. Is this really happening? Unfortunately, I’ve seen cases where this can and does happen.
The workers’ compensation attorneys at the Law Offices of James Scott Farrin can help you fight the insurance company if they try to pull any of these stunts. We know the law, we know how to try to protect your rights to medical treatment, and we have the tools, technology, financial resources, and know-how to try to get you the medical treatment you need.
But don’t wait to see if the insurance company denies your care. You need medical treatment when your doctor orders it, not after the insurance company delays.
One way to show the insurance company that you mean business when it comes to medical treatment is to contact us today or call 1-866-900-7078 so we can discuss working together to fight for your rights. Your case evaluation is completely free.
P.S. Here are more reasons to hire a workers’ comp lawyer about your claim.
You May Also Be Interested In
Why Would Your Workers’ Comp Claim Be Denied? Learn Where Things May Have Gone Wrong
Your Workers’ Comp Claim Has Been Denied. Now What?
What to Do If Denied a Second Opinion for Workers’ Comp
I’ve Been Given a Workers’ Comp Rating. Should I Close My Case?